
Yellow fever is a serious viral disease found in tropical and subtropical regions—primarily in Africa (90% of cases), as well as in South and Central America. It does not occur in Asia. Annually, an estimated 84,000–170,000 people fall seriously ill, and 29,000–60,000 die from yellow fever globally (WHO).
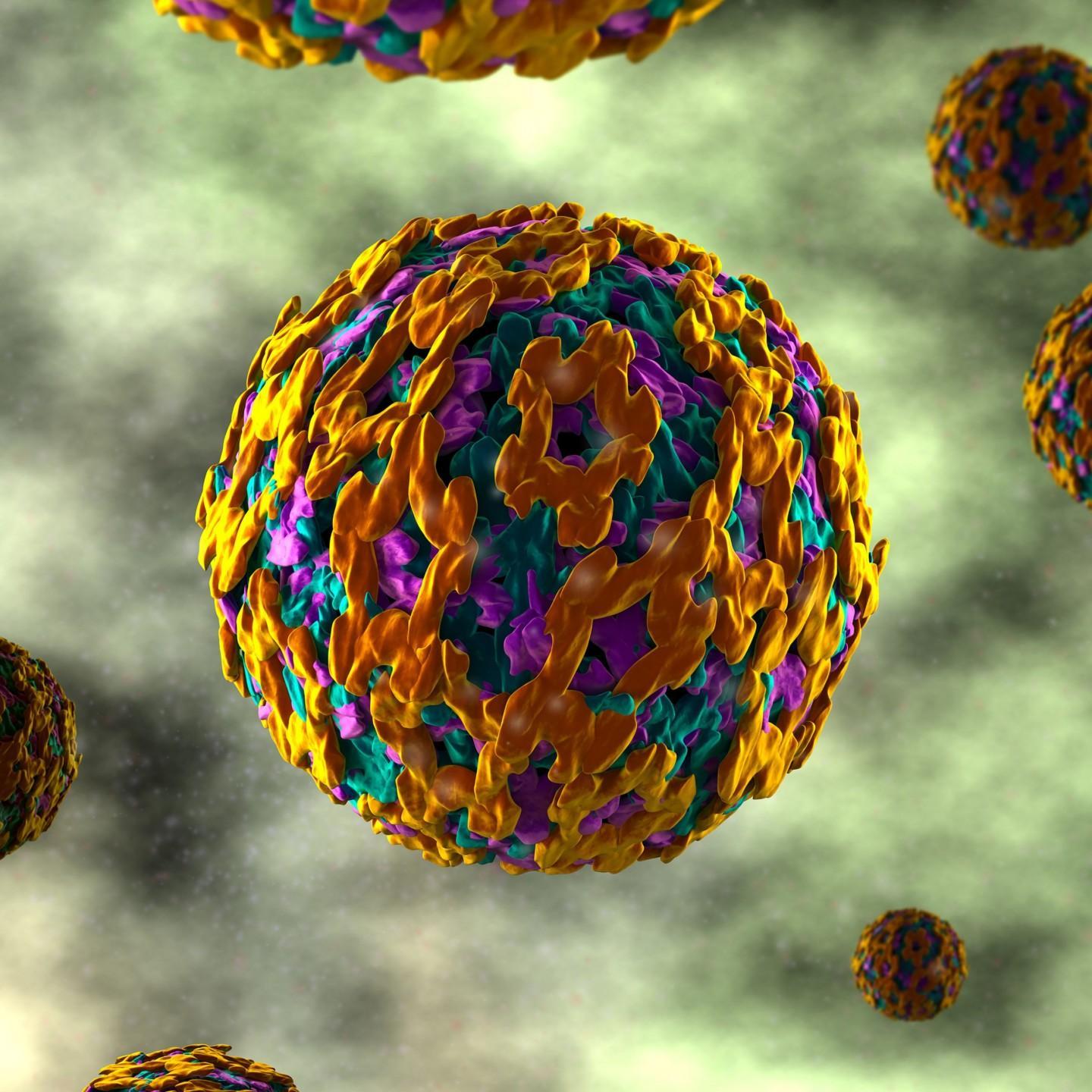
The yellow fever virus is an RNA virus and a member of the flavivirus family, related to the viruses behind Japanese encephalitis, Zika, and West Nile. Its primary hosts are monkeys. Transmission to humans doesn't occur directly from animals—or between humans — but rather through vector bites, chiefly by day-biting mosquitoes (Aedes aegypti and Haemagogus) that pass the virus from monkeys to humans or, in urban settings, from person to person.
Yellow fever typically emerges 3–6 days after a mosquito bite. Early symptoms include fever, nausea, headache, light sensitivity, lower back and leg pain, muscle aches, irritability, and dizziness. This is followed by a 2-day remission or recovery phase, during which symptoms usually subside, and many patients recover. However, around 15% of patients enter a severe "intoxication phase" with symptoms such as upper abdominal pain, jaundice (due to liver dysfunction), reduced urine output, bleeding tendencies, and multi-organ failure. In this stage, fatality rates can range from 20% to 50%.
Diagnosis is confirmed through lab tests, though early detection is difficult. Diagnosis often relies on symptom presentation combined with recent travel history to an endemic region. No specific treatment exists for yellow fever.
From the 1700s to early 1900s, yellow fever was a significant threat, with outbreaks in North America and Europe. Once the vector (Aedes aegypti) was identified and vector control efforts began, outbreaks became rare outside tropical zones. The development of two yellow fever vaccines in the 1930s led to widespread vaccination in the 1940s, drastically reducing the disease’s spread. Nonetheless, outbreaks continue to occur intermittently in endemic areas.
During 2017–2018, yellow fever expanded to new areas in Brazil—including major cities like Rio de Janeiro, São Paulo, and Salvador—though the risk remains much lower in South America compared to Africa. For unvaccinated travelers, the estimated risk of infection during a two-week visit to endemic regions in Africa is approximately 1 in 1,300 to 1 in 300, depending on the season. In Finland, only travelers are affected.
Yellow fever can be prevented through vaccination. All current vaccines contain live-attenuated virus and are highly effective—providing over 95% protection. Vaccination is recommended from 9 months of age onwards, and, according to WHO, offers lifelong immunity. It is advised for people living in or traveling to endemic areas.
However, vaccination is not suitable for immunocompromised individuals or recommended during pregnancy unless travel cannot be avoided. The vaccine virus passes into breast milk; vaccination may be considered for pregnant or breastfeeding individuals only if travel to endemic areas is unavoidable, preferably after the sixth month of pregnancy. Vaccination is not recommended for children under six months due to rare neurological risks.
The yellow fever vaccine (Stamaril®) contains a live, weakened virus strain. A single subcutaneous dose is administered, the same for adults and children. The vaccine is well tolerated, with mild side effects such as fever, muscle aches, or headache in a small minority. According to WHO, one dose provides lifetime protection, and no boosters are required.
Yellow fever poses a serious risk for people in endemic regions or travelers. Although current vaccines are effective, manufacturing them is complex and slow. To improve availability during outbreaks, FVR is researching vaccines produced with more modern methods.
Some countries — primarily in West Africa — require travelers to present a yellow fever vaccination certificate. WHO guidelines state that the certificate becomes valid 10 days after the first dose and lasts for life. This standard came into effect in July 2016; older certificates remain valid without date modifications. Only select approved healthcare centers in Finland can issue these certificates.
Additional information:
Sources:
Text updated 20.2.2024